Chronic diseases are the leading driver of U.S. health care costs, accounting for 85% of all healthcare spending. We try to direct, cajole, influence, motivate and otherwise engage with patients to get them to better self-manage their many chronic ailments. We train clinicians to treat these afflictions and invest heavily in new drugs and devices to address these primary medical challenges. Dozens of niche health services and digital health companies have sprung up to treat chronic disease, each vying to address the crisis already in play.
While we all know that far too little is spent on preventing chronic illness, one lesser acknowledged fact is how directly environmental damage and climate change drive up the increased incidence of chronic disease.
Clean air, water and food are essential to life. In a world where the air is filled with pollutants, the water and earth are filled with chemicals and plastics, and where growing healthy food and accessing drinkable water are being impeded by issues of land use and climate change, the basic building blocks of life are fast becoming health’s worst enemies.
The Health Sector’s Contribution to the Climate Crisis
It is an ironic twist that the U.S. healthcare system eschews prevention, complains loudly about the cost and human burden of chronic diseases, and yet itself generates enough environmental damage to be a significant contributor to this rising problem. Some facts to consider:
- The U.S. health care sector is the second-largest industry contributing to landfill waste worldwide
- If it were its own country, it would be the 13th largest global greenhouse-gas emitter.
- Greenhouse gas emissions from US healthcare systems rose 6% from 2010 to 2018, accounting for approximately 8.5% of all US greenhouse gas emissions.
In other words, the healthcare system is a prime cause of chronic illness directly driving up the incidence of cardiovascular conditions, respiratory ailments, cancer, and other deadly and costly diseases. Environmental causes of death, taken as a whole, are linked to 24% of deaths worldwide
Researchers have found that two healthcare sectors contributing the most to carbon emissions are hospitals (36%) and physician and clinical service providers (12%). Health systems use extensive amounts of energy, spew toxic anesthetic gasses into the air and create wastewater filled with pharmaceutical and other chemical toxins, much of which are not regulated to the extent that the damage is fully mitigated. The manufacturing, packaging and transportation practices of the pharmaceutical and medical device industries significantly compound this problem
US National Healthcare Greenhouse Gas (GHG) Emissions by GHG Protocol Scope, 2018
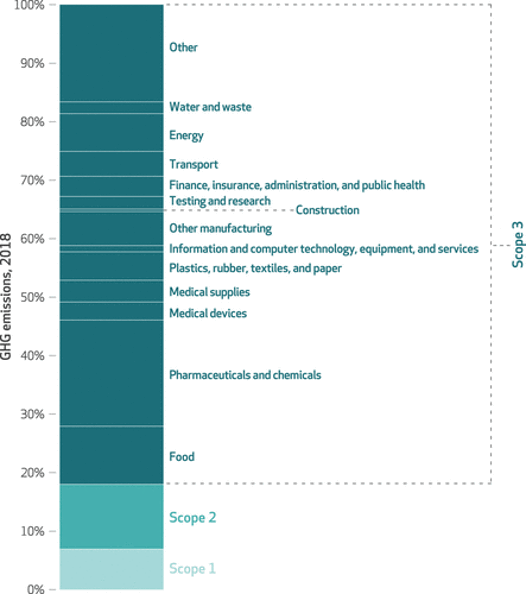
CHART NOTES: Scope 1 is direct emissions from health care facilities, Scope 2 is emissions from direct purchases of energy, and Scope 3 is all other supply-chain emissions. Source: https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.01247
In addition, the healthcare system utilizes a vast number of unrecycled plastics and other single use materials. This is the very definition of the business model of medical manufacturing and supply: make as many single-use products as possible so more of them need to be purchased (nearly every medical product is encased in plastic, not to mention the 190 billion plastic pill bottles released into the world annually, most of which are not recyclable.
It is no coincidence that the rise in chronic disease burden that started in the 1950’s is concomitant with the massive proliferation of plastics begun in that same era. When plastics leach into food and water supplies, they can have significant negative impacts on neurological, endocrine and other bodily functions. Health care’s reliance on single-use plastic materials only exacerbates these risks.
Build Healthier Communities, not Bigger Healthcare Demand
That’s one way to build market demand for healthcare services. Imagine if a tire store owner went around town popping car tires at night to build demand. While the healthcare example is not quite as pre-meditated, it isn’t that different. Every major healthcare company has an Environmental, Social and Governance (ESG) initiative, yet there is inadequate effort to address the “E”. This problem receives nowhere near the venture funding, media play or governmental attention necessary to change it.
There are solutions. The environmental damage caused by excessive plastic packaging drives up the incidence of cancer and other costly conditions. It can be no coincidence that the rise in chronic disease burden that started in the 1950’s is concomitant with the massive proliferation of plastics begun in that same era. We can reduce the use of plastics and replace them with compostable safe packaging, as is being done in the food service industry. Companies like Cabinet Health and Saatchi and Saatchi Wellness believe it’s possible to reduce plastics and replace them with compostable safe packaging, as is being done in the food service industry. The need for single use of gloves, masks, and needles are obvious, but many medical device products could be sterilized and made reusable. Unfortunately, this change is antithetical to the health of many healthcare companies stock price.
There must be greater regulation of health system, pharmaceutical and device company emissions, like that found in the Inflation Reduction Act (IRA). Yes, regulation drives up hassle and cost for healthcare companies and drives up political discontent. We know that responsive action is especially challenging when its impact seems distant, as in the case of environmental damage to patient health, although the scary objects in the mirror are seemingly much closer than they appear.
Similarly, we need a system of financial rewards for reducing carbon footprint just as there are rewards for improving patient satisfaction or reducing errors. Why not integrate environmental impact into CMS’ STAR ratings and Joint Commission metrics?
We can do all the care management in the world to try to change patient behavior, but if the healthcare systems themselves are driving up cardiovascular illness, respiratory diseases and cancer by polluting food, air and water sources, these efforts are largely pointless.
Our healthcare system is notorious for seeking ways to drive revenue now without adequate regard for the downstream impact of its actions. But if we as participants in the healthcare community are serious about our goal to improve quality and life expectancy, we need to make changes to today’s business practices to have a healthier tomorrow.
 ABOUT LISA SUENNEN
ABOUT LISA SUENNEN
Lisa Suennen has spent more than 30 years in healthcare as entrepreneur, operating executive, venture capitalist and strategy consultant. She has worked broadly across most segments of healthcare. Lisa currently leads Venture Valkyrie Consulting. Previously she has held executive-level operating roles at Canary Medical, Merit Behavioral Care and Manatt, Phelps & Phillips. She has held General Partner roles at Manatt Venture Fund, Psilos Group and she also led GE Ventures’ healthcare venture fund. Lisa founded CSweetener, a company focused on matching mentors with rising healthcare leaders (sold to HLTH Foundation).
Lisa chairs the Advisory Boards of the NASA -funded Translational Research Institute for Space Health and the International Investment Committee of the Australian government-funded ANDHealth Digital Health Fund. She is a Fellow of the Aspen Institute’s Health Innovators Fellowship and on faculty at the UC Berkeley Haas School of Business. Lisa is also the author of the Venture Valkyrie blog and is an internationally recognized writer and speaker.
Lisa is a Fellow in the first class of the Aspen Institute’s Health Innovators Fellowship. Learn more about the program and their mission to develop a community of energized, values-driven leaders committed to finding viable solutions to address U.S. health care’s problems.

